Unfortunately, due to the health of our team, Mast Cell Hope has closed down in December of 2023. We will be maintaining this site for educational purposes for as long as we can. Visit our education page for learn about mast cell disease.

Learning Resources
LIVING WITH MAST CELL DISEASE - TRIGGERS & SYMPTOMS
People living with mast cell disease can experience mast cell activation when exposed to one or more triggers. An important part of managing a mast cell condition is avoiding known triggers.The contributors that cause mast cell activation for a patient can change over time. Patients may react to something that previously was not a trigger for them at any moment, including medications.
Triggers for Mast Cell Activation1-7
Environmental
- Sudden changes in temperature, extreme heat, or extreme cold
- Strong smells/odors/fragrances
- Friction on the skin (e.g. massage)
- Vibration
- EMF (electromagnetic frequency)
- Mold
- Venom from insect stings (most notably from hymenoptera stings or the numerous species of insects that include wasps, bees, hornets, and ants)
- Heavy metals
- Sunlight
Food and beverages
- Food and beverage triggers can include any food or beverage
Mast Cell Hope tip: Each patient has different food and beverage triggers, and even low histamine foods can still be a trigger. The only way for a patient and their physician to find out what foods and beverages trigger mast cell episodes is to conduct careful food trials under close doctor supervision.
Medications
-
Antibiotics
- Vancomycin Mast Cell Hope tip: Vancomycin is a known mast cell trigger and should be avoided unless absolutely needed
- Opioids
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- Neuromuscular junction blocking agents
- Local anesthetics
- In some cases, aspirin (Warning: Never trial aspirin unless directly supervised by a physician. Aspirin can either help someone or cause anaphylaxis. For this reason, doctors recommend that patients are hospitalized when trialing aspirin.
Mast Cell Hope tip: Each patient is different and all drugs should be trialed under close supervision with a physician.
Pathogens
- Infections caused by bacteria, viruses, and parasites
- Infections caused by mycotoxins from mold
Stress
- Emotional (feelings of overwhelm and trouble concentrating)
- Physical (fatigue)
- Social (stress associated with a person’s relationships with others)
Note: This is not a complete list of triggers of mast cell activation.
Symptoms of Mast Cell Activation8-14
When mast cell activation occurs, mast cells release mediators that are known to cause a wide range of symptoms that can affect one or more organ systems.
Dermatologic (Skin)
- Pruritis (itchy skin)
- Angioedema (swelling in the deep layers of the skin)
- Dermatographia (“skin writing”)
- Flushing
- Pruritus/urticaria (hives)
- Urticaria pigmentosa (dark, itchy patches of skin that are tan or brown in color)
Respiratory (Lungs)
- Asthma
- Wheezing
- Cough
- Dyspnea (difficulty breathing)
- Swelling of the throat
Cardiovascular (Heart)
- Chest pain (non-anginal or not associated with a heart attack)
- Hypotension (low blood pressure)
- Hypotensive syncope (fainting)
- Tachycardia (faster-than-normal heart rate, while at rest)
- Arrhythmia (abnormal heartbeat)
- Kounis syndrome
Gastrointestinal (Gut)
- Diarrhea
- Abominable pain
- GERD (gastroesophageal reflux disease)
- Bloating
- Nausea/vomiting
Musculoskeletal (Muscles & Bones)
- Bone/muscle pain
- Osteoporosis/osteopenia (loss of bone mass)
Neurologic (Nervous System)
- Headache
- Brain fog
- Anxiety
- Depression
- Peripheral neuropathy (damage to the nerves located in the peripheral areas of the body, such as the hands and feet)
- Pain similar to that of fibromyalgia
Naso-ocular (Nose & Eyes)
- Nasal congestion
- Sinusitis (inflammation of the sinuses)
- Teary eyes
Systemic (Whole Body)
- Weight loss
- Asthenia (fatigue)
- Anaphylaxis
Lymphatic System
- Adenopathy/adenitis (inflammation of the lymph nodes)
Note: This is not a complete list of symptoms of mast cell activation.
When Is Mast Cell Activation Considered Anaphylaxis?
Mast cell activation symptoms can change quickly to suddenly and rapidly become anaphylaxis. Symptoms of anaphylaxis may develop after exposure to a known or unknown trigger:15-17
- Rash/hives
- Swelling in different areas of the body
- Swelling of the throat that makes it hard to breathe and/or swallow
- Coughing and or wheezing
- Tachycardia (increased heart rate of more than 100 beats per minute)
- Diarrhea, vomiting, and/or cramps
- Hypotension (low blood pressure) and/or fainting or passing out
- Tightness of the chest
- Feeling of dread or “impending doom”
Learn more about emergency treatment.
Grading System for Anaphylaxis Severity
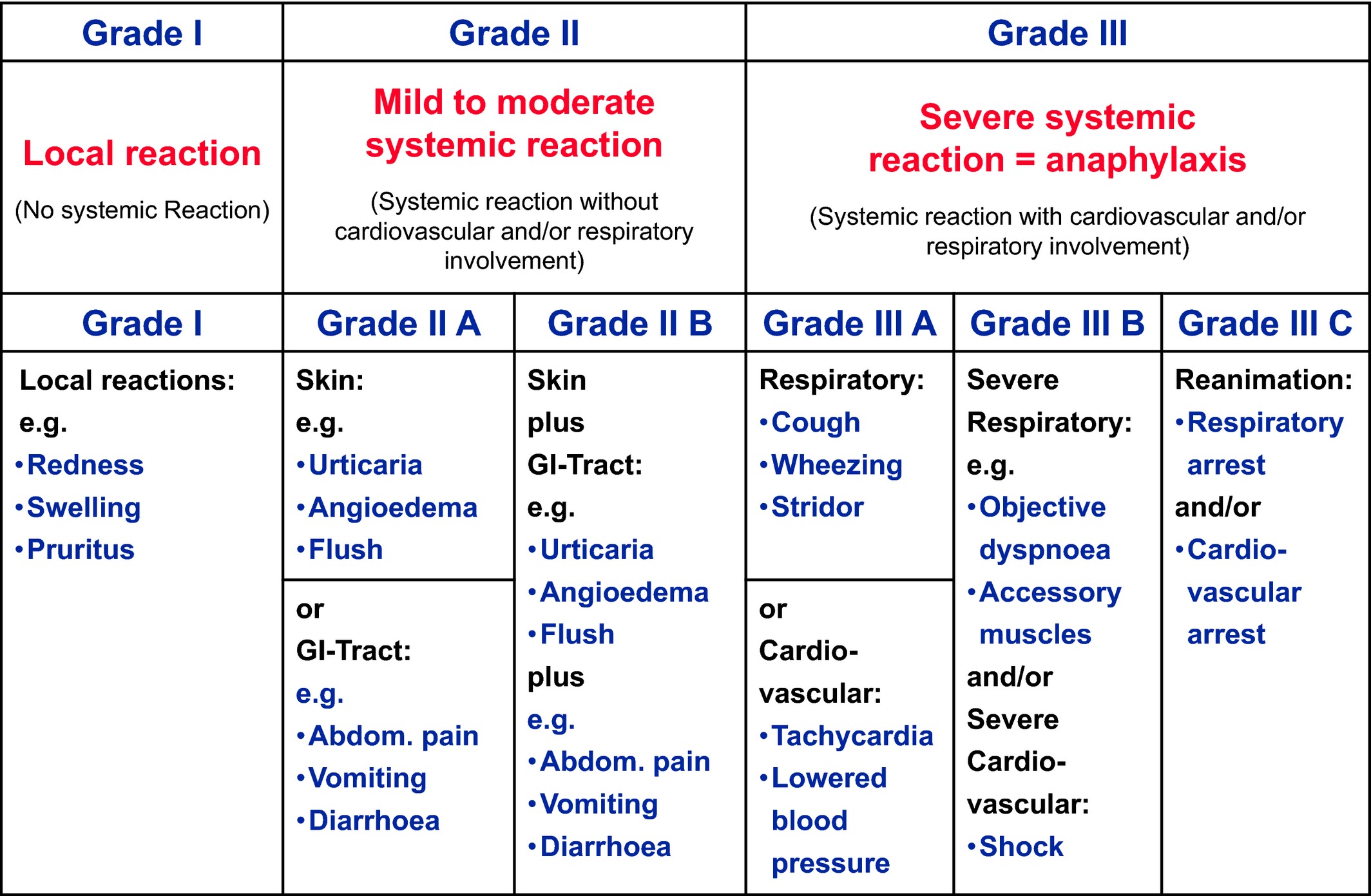
Source: Niggemann B, Beyer K. Time for a new grading system for allergic reactions? Allergy. 2016 Feb;71(2):135-6. https://onlinelibrary.wiley.com/doi/full/10.1111/all.12765
References:
- Theoharides TC, Tsilioni I, and Ren H. Recent advances in our understanding of mast cell activation – or should it be mast cell mediator disorders? Expert Rev Clin Immunol. 2019;15(6):639–656. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7003574/
- Hamilton MJ, Hornick JL, Akin C, Castells MC, Greenberger NJ. Mast cell activation syndrome: a newly recognized disorder with systemic clinical manifestations. J Allergy Clin Immunol. 2011;128(1):147-152.e2. https://pubmed.ncbi.nlm.nih.gov/21621255/
- Sarchio SNE, Kok LF, O'Sullivan C, Halliday GM, Byrne SN. Dermal mast cells affect the development of sunlight-induced skin tumours. Exp Dermatol. 2012;21(4):241-8. https://pubmed.ncbi.nlm.nih.gov/22276860/#:~:text=While%20mast%20cells%20are%20best,remodelling%20and%20pro%2Dangiogenic%20factors
- Boyden SE, Desai A, Cruse G, Young ML, Bolan HC, Scott LM, Eisch AR, Long RD, Lee CC, Satorius CL, Pakstis AJ, Olivera A, Mullikin JC, Chouery E, Mégarbané A, Medlej-Hashim M, Kidd KK, Kastner DL, Metcalfe DD, Komarow HD. Vibratory Urticaria Associated with a Missense Variant in ADGRE2. N Engl J Med. 2016 Feb 18;374(7):656-63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4782791/
- Hamilton MJ. Nonclonal Mast Cell Activation Syndrome: A Growing Body of Evidence. Immunol Allergy Clin North Am. 2018;38(3):469-481. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6049091/
- Johansson O, Gangi S, Liang Y, Yoshimura K, Jing C, Liu PY. Cutaneous mast cells are altered in normal healthy volunteers sitting in front of ordinary TVs/PCs--results from open-field provocation experiments. J Cutan Pathol. 2001 Nov;28(10):513-9. https://pubmed.ncbi.nlm.nih.gov/11737520/
- An SY, Hwang EK, Kim JH, et al. Vancomycin-associated spontaneous cutaneous adverse drug reactions. Allergy Asthma Immunol Res. 2011;3(3):194-198. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3121061/
- Theoharides TC, Tsilioni I, and Rene H. Recent advances in our understanding of mast cell activation – or should it be mast cell mediator disorders? Expert Rev Clin Immunol. 2019;15(6):639-656. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7003574/
- Jennings SV, Slee VM, Finnerty CC, Hempstead JB, Bowman AS. Symptoms of mast cell activation: The patient perspective. Ann Allergy Asthma Immunol. 2021 Oct;127(4):407-409. https://www.annallergy.org/article/S1081-1206(21)00494-4/fulltext#relatedArticles
- Pal S, Nath S, Meininger CJ, Gashev AA. Emerging Roles of Mast Cells in the Regulation of Lymphatic Immuno-Physiology. Front Immunol. 2020;11:1234. https://www.frontiersin.org/articles/10.3389/fimmu.2020.01234/full
- Cruse G, Bradding P. Mast cells in airway diseases and interstitial lung disease. Eur J Pharmacol. 2016;778:125-138. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4637266/
- Pardanani A. Systemic mastocytosis in adults: 2017 update on diagnosis, risk stratification and management. Am J Hematol. 2016;91(11):1146-1159. https://onlinelibrary.wiley.com/doi/10.1002/ajh.24553
- Wang Q, Lepus CM, Raghu H, et al. IgE-mediated mast cell activation promotes inflammation and cartilage destruction in osteoarthritis. Elife. 2019;8:e39905. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6516833/
- Kounis NG, Mazarakis A, Tsigkas G, Giannopoulos S, Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011;7(6):805-24. https://pubmed.ncbi.nlm.nih.gov/22050066/#:~:text=Kounis%20syndrome%20is%20the%20concurrence,a%20'ball%20of%20thread'
- American Academy of Allergies, Asthma, & Immunology. Anaphylaxis: Symptoms & Diagnosis. Publication date unknown. https://www.aaaai.org/conditions-treatments/allergies/anaphylaxis
- Fischer D, Vander Leek TK, Ellis AK, and Kim H. Anaphylaxis. Allergy Asthma Clin Immunol. 2018; 14(Suppl 2): 54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6156836/
- Niggemann B, Beyer K. Time for a new grading system for allergic reactions? Allergy. 2016;71(2):135-6. https://onlinelibrary.wiley.com/doi/full/10.1111/all.12765