Unfortunately, due to the health of our team, Mast Cell Hope has closed down in December of 2023. We will be maintaining this site for educational purposes for as long as we can. Visit our education page for learn about mast cell disease.

Learning Resources
EMERGENCY TREATMENT AND CARE
The most life-threatening symptom of mast cell disease is anaphylaxis. Anaphylaxis is a severe, systemic allergic reaction that comes on suddenly and can be fatal. Anaphylaxis occurs after the patient has come into contact with a possible or known trigger. Recognizing the symptoms of anaphylaxis and administering treatment early are essential to reducing the risk of death.How Can You Identify an Anaphylaxis Episode?
Both patients and physicians need to be able to identify the signs of anaphylaxis.
The most common signs of anaphylaxis are cutaneous (skin) symptoms, including:1
- Urticaria (hives)
- Angioedema (swelling of the deeper layers of the skin, most commonly in the eyes, lips, face, and genitals)
- Erythema (a rash characterized by red raised “bulls-eye” welts)
- Pruritus (itchy skin)
However, not everyone who suffers from anaphylaxis will have skin reactions. Other parts of the body that are affected by anaphylaxis include the:1,2
Throat
- Itchiness
- Swelling of the throat
Lungs
- Dyspnoea (difficulty breathing)
- Stridor (wheezing due to narrowed airways)
- Apnoea (ceased breathing)
Heart
- Tachycardia (faster-than-normal heart rate or a heart rate over 100 beats per minute)
- Hypotension (sudden drop in blood pressure)
- Cardiac arrest
- Dizziness or disorientation
- Fainting or collapsing
Mouth
- Itchiness
- Swelling of the lips and/or tongue
Gut
- Abdominal Pain
- Nausea and/or vomiting
- Diarrhea
The signs of anaphylaxis can vary widely and can be unpredictable. The severity of symptoms can change rapidly. Since anaphylaxis is a systemic reaction, it can affect one or more organ systems, including the skin, the respiratory system, the cardiovascular system, and the neurological system.
Grading System for Anaphylaxis Severity
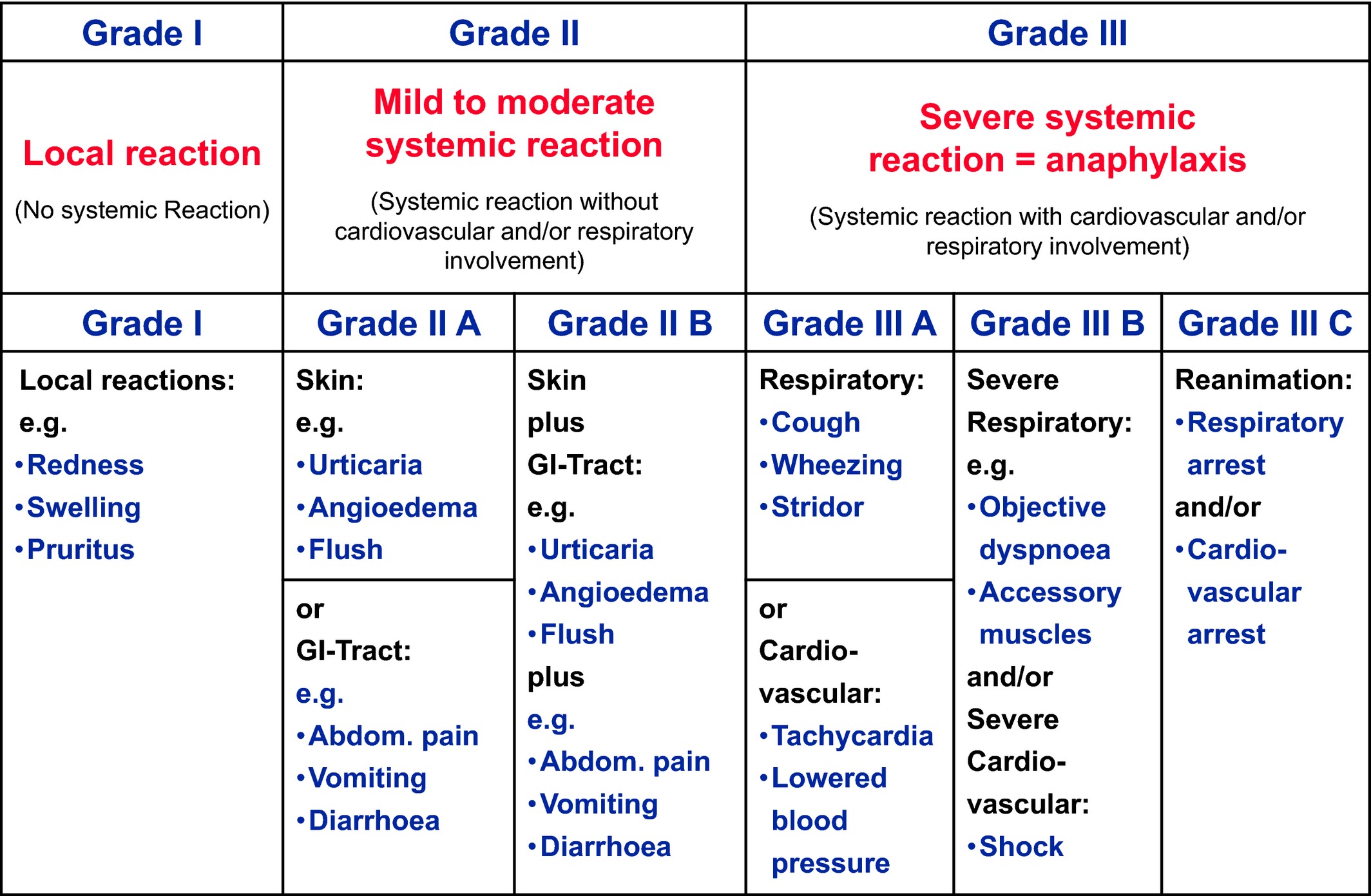
Source: Niggemann B, Beyer K. Time for a new grading system for allergic reactions? Allergy. 2016 Feb;71(2):135-6. https://onlinelibrary.wiley.com/doi/full/10.1111/all.12765
It is very likely that a patient is experiencing an anaphylactic episode if they present with one of the three following criteria:1
-
An anaphylactic-like response that occurs suddenly and involves the skin, the mucosal tissue (i.e. the mouth, nose, gut, and lungs), or both, in addition to one of the following symptoms:
-
Respiratory distress
- Difficulty breathing
- Wheezing
- Hypoxemia (lower-than-normal levels of blood oxygen)
-
Hypotension or symptoms of end-organ damage
- Incontinence
- Syncope (loss of consciousness)
- Hypotonia (collapsing)
-
-
Symptoms that affect two or more of the following bodily systems after exposure to a likely trigger:
- Skin
- Heart
- Brain (neurological)
- Lungs
- Gastrointestinal tract (gut)
-
Hypotension or symptoms of end-organ damage
- Incontinence
- Syncope (loss of consciousness)
- Hypotonia (collapsing)
-
Hypotension that comes on after exposure to a known trigger (note: some patients exhibit severe hypertension):
- For infants and children, this refers to low systolic blood pressure according to the child’s age or a greater than 30% decrease in systolic blood pressure from the child’s norm.
- For adults, this refers to a systolic blood pressure reading of less than 90 mmHg or a greater than 30% decrease from the individuals’ norm.
Self-Treatment of Anaphylaxis
Mast Cell Hope tip: All patients should create an emergency plan with their physician that may include:
- Increasing H1 and H2 blockers
- Taking Benadryl®
- Using an inhaler
-
Using a self-injectable Epi-Pen®
The patient’s close friends and family members should be properly trained on the use of epinephrine auto-injectors.
Seek medical attention immediately after administering epinephrine. As much as 15% of anaphylactic episodes are considered recurring, meaning that patients could experience a second wave of symptoms.1 Patients will also likely need additional treatment following epinephrine administration to manage symptoms of anaphylaxis.
Anaphylaxis Action Plan
Patients diagnosed with mast cell disease should work with their physicians to create an emergency treatment plan to be executed before going to the hospital. This plan should be carried with patients at all times.
An anaphylactic treatment plan should include:1
Contact information
- Emergency contact information: family members and the patient’s doctors
- Contact information for a local ambulance or emergency services
The signs of anaphylaxis
- How to identify an anaphylactic episode
Triggers (allergens)
- Triggers (allergens) that should be avoided, including any medications (both generic and brand names of all medication allergies)
Prescribed medications and how they should be used
- Epinephrine auto-injector pen (with detailed instructions on how to administer–with pictures if possible)
- Antihistamines
- Inhaler (inhaled beta-2 agonists for asthma or bronchospasms)
Where these medications are stored
- Especially when the patient is at home, school, or work.
References:
- Fischer D, Vander Leek TK, Ellis AK, and Kim H. Anaphylaxis. Allergy Asthma Clin Immunol. 2018; 14(Suppl 2): 54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6156836/
- Poziomkowska-Gęsicka I and Kurek M. Clinical Manifestations and Causes of Anaphylaxis. Analysis of 382 Cases from the Anaphylaxis Registry in West Pomerania Province in Poland. Int J Environ Res Public Health. 2020;17(8):2787. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7215547/